Physician Adoption of AI Will Radically Change the Role of Pharma Marketers
/Success in the future requires conceptualizing how AI will transform their customers, their brands, and their future role
The goal of pharmaceutical marketing is to ensure that a physician has top-of-mind brand awareness at the moment that the right patient is in their office and it's time to write a prescription.
The effectiveness of pharmaceutical marketing in driving physician prescribing is well-established, supported by everything from gut feeling to market research studies to rigorous academic publications. And while specific channels and tactics have evolved over time, the general formula that drug companies follow in order to convince a physician to prescribe a given product for an appropriate patient has remained unchanged for decades; start with good clinical data, craft a compelling positioning, create a motivating campaign, and target the right prescriber.
Effective marketing works by getting inside the mind of the customer, understanding how they make decisions, and inserting the brand into their decision-making process. But what will happen when the bulk of that decision-making process occurs by way of an Artificial Intelligence computer algorithm rather than in the mind of the customer?
The decision-making process a physician goes through when selecting the appropriate prescription drug for a specific patient requires processing a dizzying array of variables.
There are SSRIs and SNRIs, CCBs and ACEs and ARBs, GLP-1s and SGLT-2s
There are agonists and antagonists and blockers and inhibitors
There are 2nd and 3rd and Nth generation products
There are CRs and ERs and XRs and SRs
Are there any co-morbid conditions in the picture?
Which concomitant meds is the patient taking?
What is the patient’s BMI? A1C? FEV1? LDL? GFR? BUN? FBS? HCT? LFT? ETC?
Then layer on the multiplicity of branded and generic options within each class, each with its own unique properties, clinical data, dosing, side-effect profiles, and other idiosyncrasies. It’s easy to see that coming to a treatment decision can be a daunting task. And sometimes a thankless one.
If At First, You Don’t Succeed…
Treatment guidelines and clinical experience (and pharmaceutical marketing efforts) may help doctors navigate through the various choices. But all-too-often, prescribers and patients are frustrated when a lack of efficacy or bothersome side effects require them to abandon whichever drug has been initially prescribed and start all over with another agent.
For example, in the STAR*D trial (Sequencing Treatment Alternatives to Relieve Depression), the largest and most consequential study of depression treatment, fewer than 1-in-3 patients achieved effective/tolerable symptom control with the first antidepressant prescribed.
Similar results - or lack thereof - are seen in the treatment of most chronic conditions (including diabetes, hypertension, psoriasis, arthritis, COPD, and others) impacting hundreds of millions of Americans and hundreds of thousands of prescribers.
Great Expectations
Given that the current "treatment guidelines and clinical experience" in many disease states are known to be less effective in choosing the right drug than tossing a coin… isn’t it reasonable to expect that both patients and prescribers will embrace an improved, evidence-based approach to prescribing that has been demonstrated to effectively match an individual patient with the best medication for them?
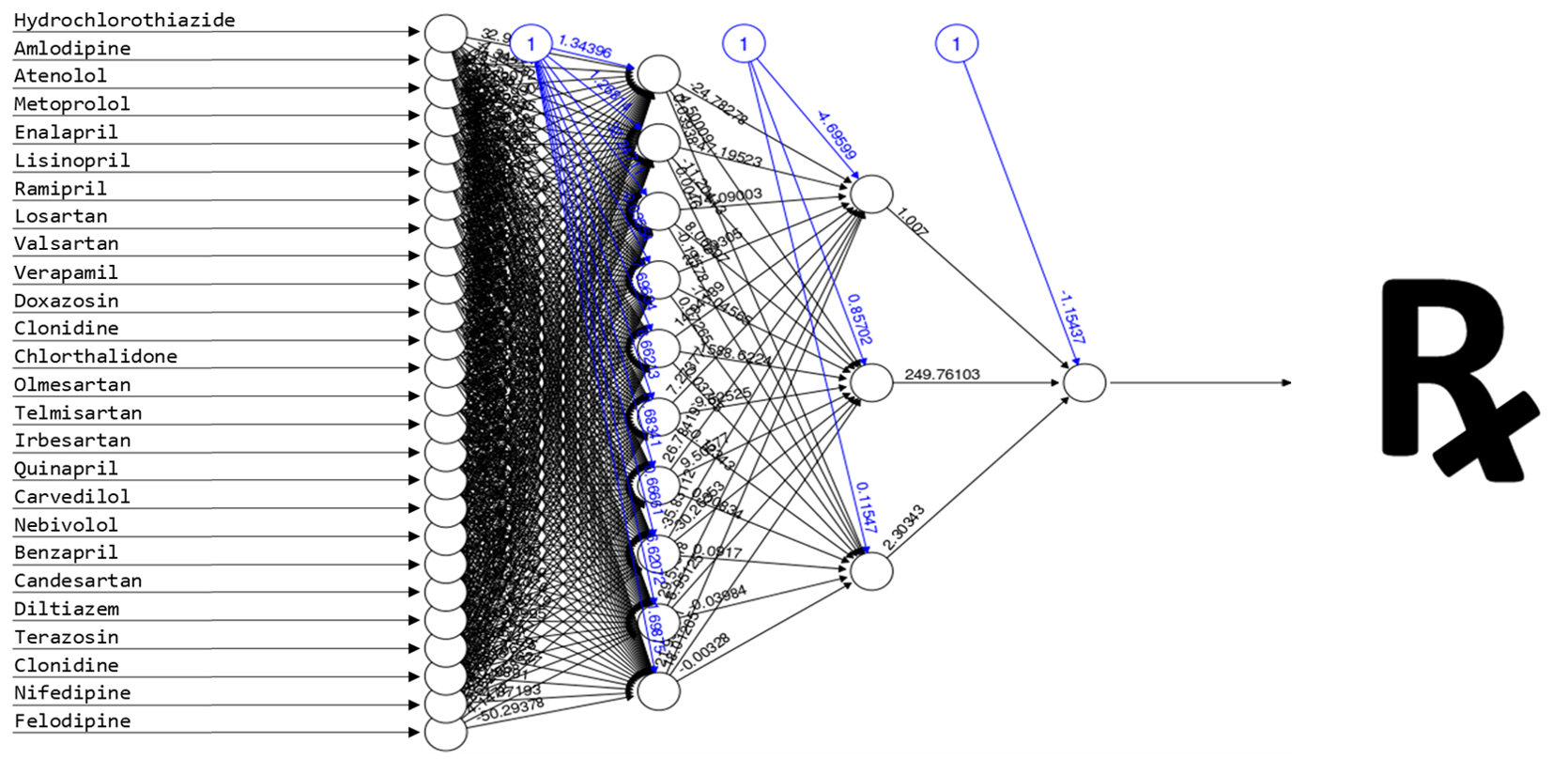
AI uses advanced algorithms to analyze information and provide solutions. While it’s impossible for busy physicians to consider ALL possible options or process the sheer volume of available data when choosing a medication, with machine learning… the more options and data the better.
This is precisely what artificial intelligence offers. And patients and prescribers alike fully expect to reap such benefits from the application of AI to healthcare decision-making.
Nearly two-thirds of patients look forward to AI-enabled healthcare, according to Accenture’s 2018 Consumer Survey on Digital Health
A majority of patients in another survey report they are at ease with the coming adoption of AI in healthcare; more so than in any other use case.
85% of physicians expect patient care will benefit from digital health technologies such as artificial intelligence, according to a survey conducted by the American Medical Association
Nearly 88% of physicians surveyed in 2017 believe that AI will improve overall care, and 83% anticipate more accurate diagnostic and treatment decisions.
Indeed, more than half of healthcare professionals surveyed believe that “widespread adoption” of AI is less than five years away, and close to 20 percent believe it will take less than two years to reach full-scale adoption. And as AI technology continues to advance, they have every reason to be optimistic.
Rise Of The Machines
Currently, most medical decisions are made using a case-by-case, experience-based approach. But there is a growing body of evidence that many diagnostic and treatment decisions - including prescribing of medications - might be best handled through rigorous analytical modeling rather than clinician intuition alone. Hardly a day goes by without news regarding the potential of AI to improve diagnosis of vexing medical conditions; recent articles about the diagnostic prowess of AI covered everything from mental health to skin cancer to retinal disease to Parkinson’s disease and dementia.
And once a diagnosis is made, AI promises similar improvement in treatment decisions. According to one AI researcher, “with the increasing availability of electronic health records, health information exchanges, large public biomedical databases, and machine learning algorithms AI promises to personalize treatment through integration of diverse, large-scale data passed along to clinicians at the time of decision-making for each patient.”
Let’s stick with antidepressant therapy as an example. AI researchers at Yale, starting with 164 variables in the STAR*D trial data set, identified 25 key factors that are predictive of treatment outcome in depression. The machine learning algorithm they developed accurately predicted a first-course-of-therapy success rate as high as 64.6%; nearly twice that seen in clinical practice (<35% in STAR*D.) (Cross-trial prediction of treatment outcome in depression: a machine learning approach. Chekroud, et al; Lancet, 2017)
As early as 2013, researchers at Indiana University had developed a machine learning model that matched patients with the specific antidepressant that is best for them, predicting a >40% improvement in treatment outcomes, and nearly a 60% reduction in treatment costs, compared to physician-selected treatment. Not surprisingly, similar results have been seen in nearly every situation in which AI-driven prescribing algorithms have been applied.
What The Future May Hold
But how can we determine what impact Artificial Intelligence will have on pharma marketing down the road? According to Amara’s Law, there is usually a tendency to overestimate the impact of new technology in the short run… and underestimate its impact in the long run.
All of which begs the question: How will the role of the pharma marketer be impacted in a world where the analysis and decision-making process behind prescribing decisions no longer occurs solely in the mind of the customer?
Who will be the key customer in an AI world? Somewhat tongue-in-cheek, but will the target customer be the prescriber, the patient, the payer, or... the programmer? Sure, in the near term, physicians may have the final say; able to "overrule" the drug selected by an AI prescribing platform. But will they? And if so... for how long? We’ve seen how quickly prescribers are willing to accommodate payer influence - another group that is eagerly anticipating AI’s ability to improve outcomes and drive down costs - when the payer’s desired agent is also supported by the clinical data. The application of AI to healthcare in general - and prescribing decisions specifically - is not science fiction. It's just science. Good science. Physicians will see that. Quickly. Far more often than not, an evidence-based, data-driven AI platform will select a drug that the physician will recognize and accept as an appropriate - if not the best - drug for the patient. Physicians are rapid adopters of technology that makes them better doctors. There is little doubt that AI-driven prescribing will make them better doctors.
What data will be needed to launch a minimally viable product in an AI world? The data needed to gain FDA approval and create sales materials that a representative can use to try to influence a single prescriber is very different from the body of data needed to influence a "big data" driven AI model. It's hard to imagine a Phase III trial for a new antidepressant that looks at the 25 variables the Yale AI model found to be predictive of better treatment outcomes. How diverse a patient population will be needed in trials? Not just gender, race, age, etc. How about BMI or marital status? Diet and exercise levels? What about co-morbid conditions? Concomitant drugs? A dozen different lab values and ranges? An AI model that's been trained on real-world data from >100,000,000 patient-years of therapy with amlodipine, lisinopril, valsartan, metoprolol, hydrochlorothiazide, etc, etc, may have a hard time finding an appropriate place for a new anti-hypertensive agent supported by data from a relative handful of "otherwise healthy" patients in two non-inferiority trials.
How will data generated by post-launch clinical experience impact the brand in an AI world? The benefit of machine learning models is that they learn. They will not simply hard-code the data from exquisitely well-designed and adequately controlled pivotal trials. A dynamic AI platform will be able to begin pulling in EHR, pharmacy claims, and demographic data about real world patients treated with a newly launched product. The specific patient type asked for in marketing efforts has always played a role in the success of a brand. In a world where AI "sees all, knows all, tells all" the influence of appropriate patient selection will be even more critical, as the clinical results seen in those patients - good and bad - will be pulled right back into the model. There’s a high likelihood that an AI algorithm might re-position, niche, or completely disregard a given brand before anyone even realizes it’s happened.
Where will AI-driven prescribing algorithms have the greatest impact? When AI prescribing platforms are fully validated and broadly embraced, there may well be disease states, therapeutic categories, drug classes, or even entire patient populations in which prescribing decisions are essentially rendered impervious to marketing efforts. How much - and how soon - will the playing field change? Will relatively low-interest/low-involvement categories be hit soonest? Or will physicians, patients, and payers first look to the power of AI in more complex, high-stakes prescribing situations? Is it fair to assume that brands with limited clinical differentiation - or limited datasets - will be hit hardest? How will this dynamic impact current brands? Compounds in development?
The answers may not be obvious just yet, as AI technology, its role in healthcare specifically, and society in general continues to evolve. But what is clear is that now is the time for pharma marketers to start asking the questions. And doing so requires more than a passing familiarity with Artificial Intelligence. Grasping the strategic implications of AI for our business requires marketers who have a foundational understanding of the genuine promise of AI technology… and are able to conceptualize how AI will transform our customers, our brands, and our future role.